Type a search + hit enter!

On a previous edition of #milkmonday, I highlighted what the WHO Code is, why it is important, and why I, as an IBCLC, fully support the implementation of the WHO Code (amongst other supportive maternity laws and practices). But the question follows: Does the WHO Code work and can it be implemented it in such […]
read more
latest post

read more
On a previous edition of #milkmonday, I highlighted what the WHO Code is, why it is important, and why I, as an IBCLC, fully support the implementation of the WHO Code (amongst other supportive maternity laws and practices). But the question follows:
Does the WHO Code work and can it be implemented it in such a large country?
To answer the second part of the question, it can be implemented in a large country. India – the country with the second largest population in the world sitting at approximately 1.4 billion – has implemented the WHO code. Not surprisingly, they also have an exclusive breastfeeding prevalence of ~55% (15% higher than the world average of 40%).
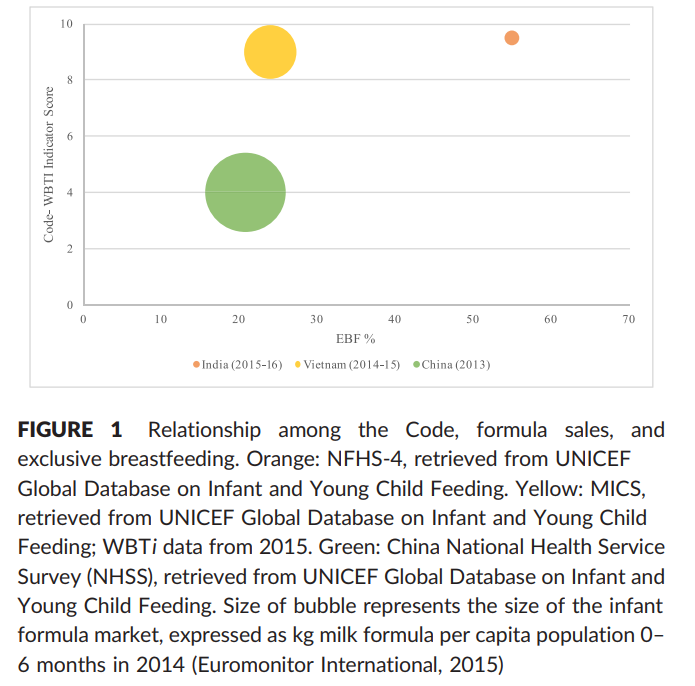
To answer the first part of the question is a little bit more complicated. Supporting exclusive breastfeeding through 6 months of age cannot be achieved by simply implementing the WHO Code. However, when a country implements the WHO Code, it speaks to the type of culture they are trying to create. A recent study out of the Yale School of Public Health represented a part of this issue visually:
In the above image you can see that China, a county that previously enforced the WHO Code, but chose to abandon their enforcement of the Code in 2017, has a much larger infant formula market (as seen by the size of the bubble) when compared to Vietnam and India. Similarly, they also have the lowest rates of exclusive breastfeeding.
The qualitative study, though, found that implementation and enforcement of the WHO Code alone was insufficient on its own to increase exclusive breastfeeding rates. Other factors that were found as necessary to increase exclusive breastfeeding rates included:
-
Six months paid maternity leave
-
Training on breastfeeding for health professionals
-
Breastfeeding-friendly hospitals
-
Pre- and in-service on The Code for health professionals (e.g. buy in)
-
Research and evaluation on The Code and exclusive breastfeeding
How will The Code be enforced?
Lucky for us in the community, the Yale School of Public Health also began to address this in the same publication, suggesting approaches for manufacturers, suppliers, sellers, and health professionals. These suggestions include proportional sanctions for all involved in the promotion and marketing of breastmilk substitutes, conflict of interest training, continual monitoring systems, and legislation around the topic.
Certainly, this publication does not offer all of the solutions necessary for increasing exclusive breastfeeding rates, but it is a great start.

read more
Medications and lactation can be a difficult topic, because there is a lot of conflicting information out there on what is safe and what should be avoided. This can be overwhelming for someone who wants to take an over-the-counter (OTC) medication to feel better but is worried about exposing his/her infant to medication. Many people […]

read more
Directly after birth we know that skin-to-skin contact had quite a few benefits for both the mother and the newborn baby. These benefits include infant temperature regulation and blood glucose control, maternal confidence in handling her infant, improved bonding between the mother and the infant, and opportunity to begin the breastfeeding relationship.
With so many benefits to both the mother and the infant, it seems that skin-to-skin contact would be standard after a birth where both mother and infant are able; however, in many hospitals this is not the case.
A 2018 study published in BMC pediatrics took a qualitative approach to see if they could identify why skin-to-skin contact is not happening in healthy neonates in a hospital in Bangalore, India. In order to do this, the researchers interviewed residents and postgraduates in obstetrics and pediatrics as well as nurses. The researchers also held focus groups to encourage discussion and uncover additional information.
What barriers were found?
Major Barriers
-
Skewed health-care staff client ratio in the labor room, which led to time constraints
-
Apprehensions related to the procedure, including a concern for the safety of the newborn
-
A lack of awareness, lack of belief in, or lack of motivation to encourage of skin-to-skin contact
Minor Barriers
-
Interference with other clinical procedures
What helped with achieving skin-to-skin contact?
-
Knowledge of the benefits, including direct motivation by a pediatrician
-
Having a dedicated staff or family member advocating for skin-to-skin
-
Maternal desire to have skin-to-skin contact
-
Initiation of early skin-to-skin contact
For providers
While this study took place in India, I believe that there is quite a bit of information that we can take and apply anywhere in the world. Speaking to your clients and their support partners about evidenced-based postpartum practices can influence the type of care they ask for and get after delivery. Teach your clients about skin-to-skin contact and the impact it can have.
For parents
This article provides evidence that advocating for yourself can make a difference in the care that is provided during your postpartum period. Make sure to have a support person (friend, spouse, family member, or anyone else you trust) who knows about your postpartum wishes and can help advocate for you after birth. If you are looking for a quick guide to the first 48 hours of your baby’s life, you can download my 2 page quick guide by clicking below!
Get Your copy →
Cross the finish line with confidence.
Don't walk into your IBCLC exam nervous - with our comprehensive study guide in your back pocket, you'll be prepared for every scenario and question.