Type a search + hit enter!

Vitamin B6, also known as pyridoxine, is a water soluble vitamin that plays an important role as a coenzyme in the human body. A coenzyme is a molecule that binds to an enzyme allowing it to function – and pyridoxine binds to many enzymes (over 100!) that are important in energy metabolism. Good food sources […]
read more
latest post

read more
Vitamin B6, also known as pyridoxine, is a water soluble vitamin that plays an important role as a coenzyme in the human body. A coenzyme is a molecule that binds to an enzyme allowing it to function – and pyridoxine binds to many enzymes (over 100!) that are important in energy metabolism. Good food sources of pyridoxine include fish, poultry and certain nuts. Many prenatal and multivitamin/multimineral supplements contain pyridoxine. Nursing women should consume ~2 mg of vitamin B6 per day.
For a nursing mother, pyridoxine in the diet is important because concentrations in breast milk are dependent on maternal intake. A landmark study completed in 1985 showed that as maternal pyridoxine intake increased, so did concentrations in human milk. Additionally, recent research has shown that B-vitamins in human milk can fluctuate daily based on time of day, dietary intake, and when vitamin supplements are consumed – so avoiding pyridoxine is not advised.
When it comes to breastfeeding, though, nursing mothers may need to be careful about how much they are taking (particularly in supplements). According to one study, supplemental doses of pyridoxine ranging from 0.5-4.0 mg/day had no impact on serum prolactin levels or milk supply. Similarly, another study saw no impact of a maternal 100 mg intramuscular dose of pyridoxine at term. There is some evidence that high doses of B6 (600 mg/day) can cause suppression of lactation. While the body of evidence is not robust, because B6 levels in milk are easily impacted, do not advise mothers to avoid pyridoxine. It may be appropriate for an RD to evaluate B6 intake to ensure it is less than 4 mg per day if you suspect B6 intake may be impacting milk supply.
Interested in nutrition support during pregnancy or lactation? Email nutrition@hopefeedsbabies.com to set up your appointment today!

read more
Cannabinoids are a class of naturally occurring, biologically active molecules. Delta-9-tetrahydrocannabinol, more commonly known as THC, is a psychoactive cannabinoid found in marijuana – this is not produced in the human body. There are cannabinoids produced by the human body (endogenous cannabinoids) that act on the endocannabinoid system (ECS) to elicit neurological responses by binding […]

read more
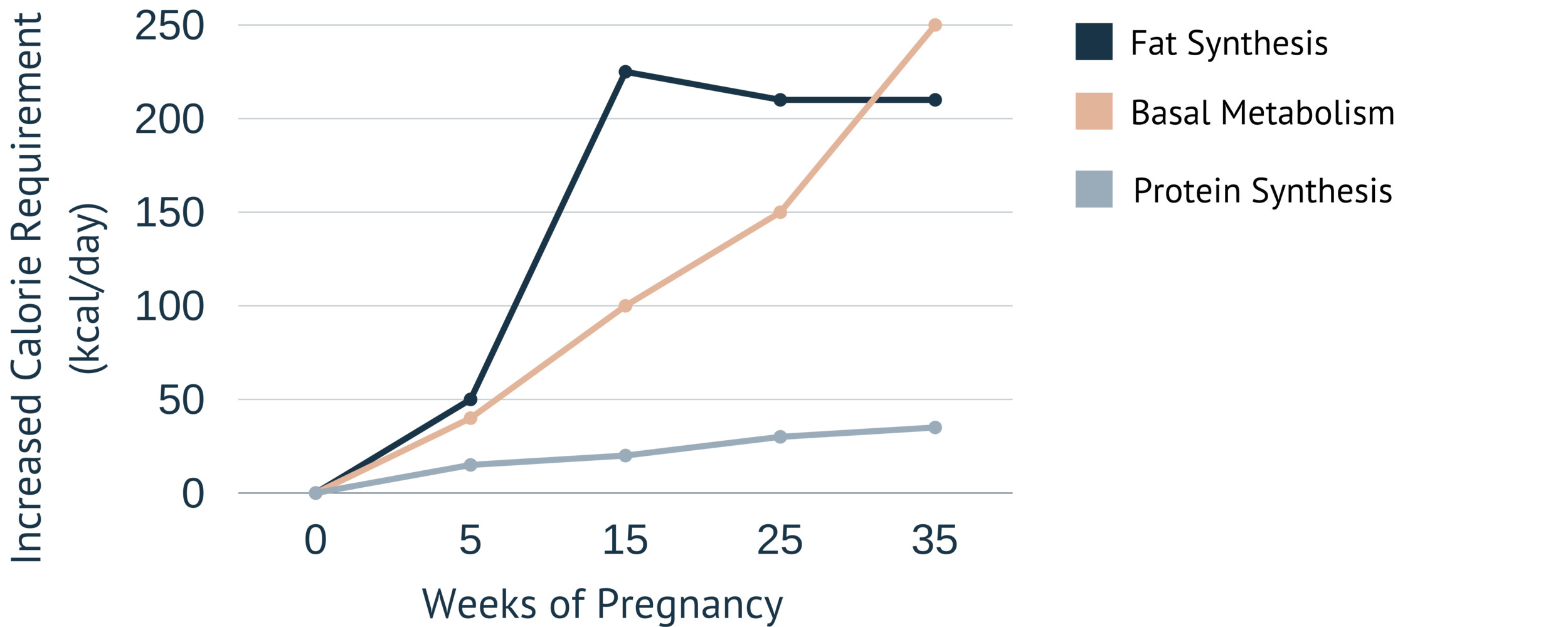
Increased hunger is a natural occurrence during pregnancy, as there is a tiny human growing. However, those energy (calorie) requirements are not of a second full-grown human. So, how much do energy requirements change during pregnancy? Let’s have a look:
As you can see in the above image, the further along in pregnancy, the higher the energy needs are. A majority of the extra calories consumed during pregnancy are used for fat synthesis. Fat synthesis is important during pregnancy, as these fat stores will be mobilized during the postpartum period to ensure adequate milk fat concentrations for the newborn. The extra calories also support tissue generation through protein synthesis in the placenta and uterus.
The weight gain guidelines from the Institute of Medicine range from 11 to 40 pounds throughout pregnancy. It is also the recommendation of the Institute of Medicine that most of that weight be gained in the second and third trimesters of pregnancy. Despite these (seemingly) specific numbers, energy needs vary from woman to woman. I always recommend that women listen to their body. Eat when feeling hungry, choosing foods high in nutrients. Drink when feeling thirsty. And remember, women know their bodies. It is our job as practitioners to remind them that they do.
Are you looking for more individualized support? Can now meet virtually with a Registered Dietitian through Hope Feeds Babies. Click below to schedule!

read more
Extended breastfeeding – or nursing a child beyond the first year of life – is becoming more common in the United States due to public health efforts to normalize breastfeeding and scientific evidence of the benefits of breastfeeding. However, policy and research are only a piece of the puzzle. Social media influencers and bloggers are […]

read more
As a nutritional biochemist, I am always interested in how we can support diet quality and food security, especially for low-income populations. Interestingly, a recent study published in the Journal of Human Lactation looked at 1,226 WIC participants found that breastfeeding duration was associated with improved diet quality for the toddler at 36 months of age. The study was a secondary analysis set up to look at within-individual associations over time. This means that rather than having any type of intervention, the researchers retrospectively analyzed data that was collected for a different study.
In order to measure the diet quality of the toddlers, the study used the USDA’s Healthy Eating Index. After conducting the phone interviews to determine the diet quality, the researchers looked back at duration of breastfeeding and found that the longer the dyad breastfed for the better the diet quality. It is important to point out that these families had nutritional support through their WIC benefits – so this speaks to the WIC program’s ability to support healthy diets for children as well.
This is not the first study to investigate the impact of breastfeeding on diet quality and similar results were found in an Australian study looking at toddler diet quality. This study found that in addition to breastfeeding status, maternal modeling of healthy eating behaviors also impacted the toddler’s diet quality.
Some studies have also looked at the interaction between breastfeeding cessation and toddler diet quality. Another study that was done in Australia found that both early breastfeeding cessation and early introduction of solids was associated with preference for energy-dense, low nutrient foods.
While we certainly don’t have a complete understanding of how children develop food preferences, we do have evidence-based recommendations that encourage children to have a healthy variety of foods in their diet:
-
Exposure: make sure your children see a variety of colors, textures, and cooking styles represented in their age-appropriate foods. Encourage your kids to put foods on their plates even if they don’t want to eat them.
-
Access: make it easy for your toddlers to access healthy foods. This can mean having appropriately sized fruits, veggies, cheese, meats, and whole grains available where they can reach them.
-
Modeling: let them see people they look up to (parents, friends, babysitters, relatives, etc.) eating foods that they may be hesitant to try.
Looking for more information about nutrition during lactation? Download my two page quick guide!

read more
Medications and lactation can be a difficult topic, because there is a lot of conflicting information out there on what is safe and what should be avoided. This can be overwhelming for someone who wants to take an over-the-counter (OTC) medication to feel better but is worried about exposing his/her infant to medication. Many people […]

read more
What you feed your baby and how it impacts their gut bacteria – scientifically termed the “microbiome” – has been a growing area of interest in the breastfeeding world. It is well established that feeding an infant cow’s milk based formula significantly changes the number of species and type of bacteria that grow in an infant’s gastrointestinal tract, and is associated with negative clinical outcomes. However, there is less research looking at the difference between receiving milk from the infant’s birth mother (termed “mother’s own milk”) or donor human milk.
Recently, a new article was published in American Journal of Clinical Nutrition that explored the differences between infants fed either donor human milk or their own mother’s milk.
What is donor human milk?
In the context of this research article, donor human milk is milk purchased from mothers who are producing too much. This milk is then screened and pasteurized (subjected to heat treatment) by Prolacta Bioscience in order to remove all bacteria. Pasteurization is important in this context because the donated milk is going mainly to premature infants who may be sick or immunocompromised. Milk banks want to ensure that there are no pathogenic bacteria or viruses that could hard these infants.
What difference does it make?
Donor human milk is different from milk that would come from an infant’s own mother for a few reasons.
-
Exposure to heat can decrease the concentration of certain micronutrients
-
Exposure to heat can decrease the activity of certain enzymes and immune compounds
-
The loss of bacteria does mean potentially harmful bacteria, but can also mean the loss of bacteria beneficial for development of the infant microbiome
What is the impact on the infant microbiome?
This new research provides evidence that infants fed a diet consisting mostly of donor human milk (average: 14% mother’s own milk) have a decreased diversity of gut microbiota in all stool samples collected over the 6-week duration of the trial.
The infant’s fed their mother’s own milk had more Bifidobacterium and Bacteroides genus bacteria than donor human milk fed infants. These bacterial species have been shown in other research to be beneficial for the growth and development of the infant when they are in the neonatal intensive care unit. Additionally, lower levels of Bacteroides bacteria have been linked to development of obesity in individuals with metabolic syndrome.
Donor human milk fed infants had more Staphylococcus genus bacteria. This genus of bacteria is known to contain pathogenic microbes. This could put the infant at an increased risk of development of illness.
Maybe most importantly, infants fed mostly their mother’s own milk (average: 91% mother’s own milk) had higher feeding tolerance than infants fed donor human milk. This is certainly important in growth and development, because the more food that the infant is tolerating, the faster they can grow.
Why is this important?
As much of my research focuses on the use of donor human milk, this article further emphasizes that donor human milk is supposed to be used specifically as a band-aid, with the goal of providing an infant their mother’s own milk. A mother’s milk is specifically designed to meet the needs of her infant. The mother’s milk contains immune components specific to that dyad’s environment, nutrition optimized for the infants age and status, enzymes to help that baby digest and absorb nutrients, and so much more. We need to do better at nurturing a culture that provides women the support and encouragement they need to feel empowered to breastfeed their baby.
Get Your copy →
Cross the finish line with confidence.
Don't walk into your IBCLC exam nervous - with our comprehensive study guide in your back pocket, you'll be prepared for every scenario and question.