Dietary Control of Subclinical Mastitis

May 20, 2021
Subclinical mastitis (SCM) is common, and while many IBCLCs have anecdotally recognized similarities between clients, a specific etiology is not well defined. Recent studies (1,2) have observed correlations between increased levels of proinflammatory cytokines and alterations in anti-inflammatory breast milk components and subclinical mastitis.
While inflammation in and of itself is necessary for our survival, a chronic proinflammatory response with no return to baseline can cause issues. Anti-inflammatory diets have been investigated for their effectiveness in resolving symptoms of chronic inflammatory diseases – such as irritable bowel disease and rheumatoid arthritis – and seen success.
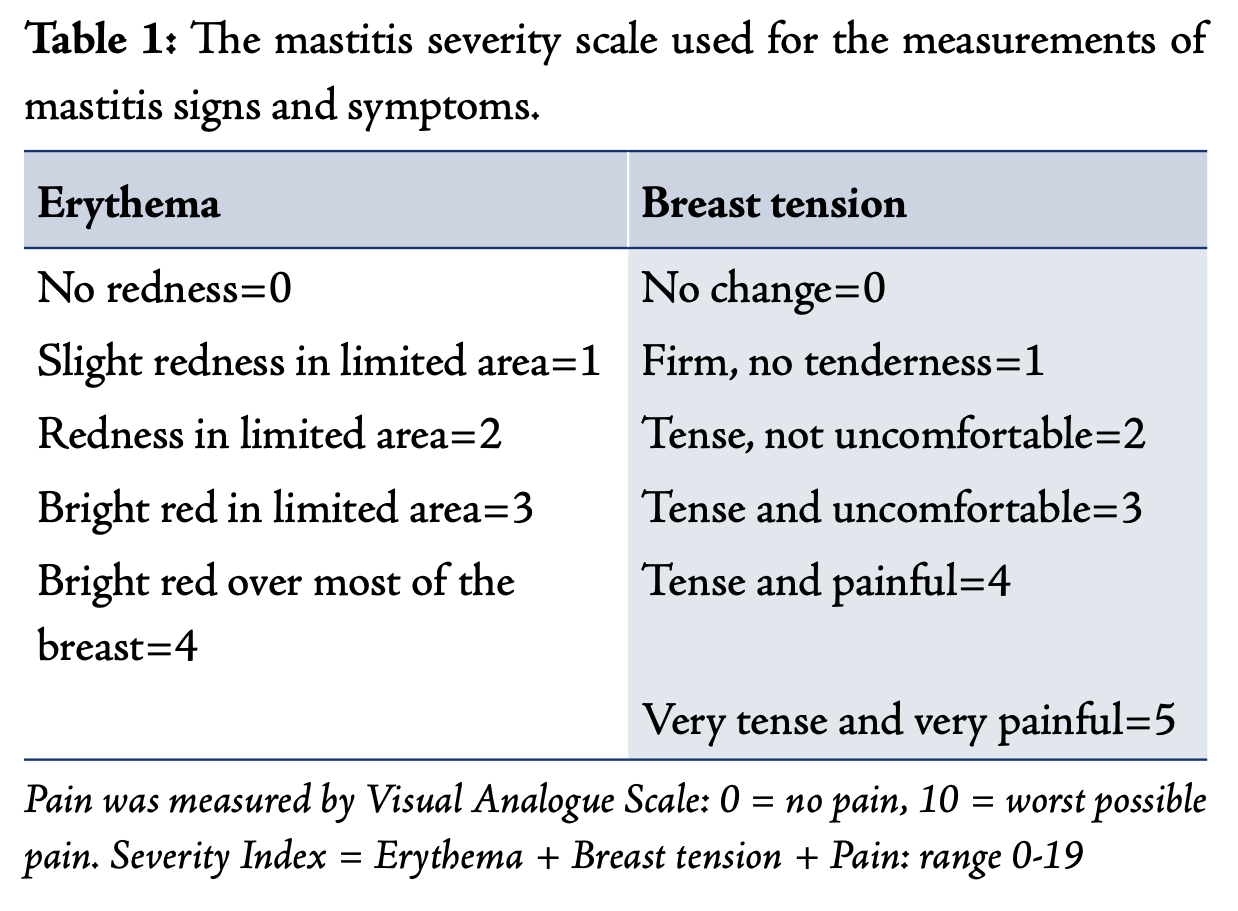
Certainly, it may be possible that subclinical mastitis is associated with a chronic pro-inflammatory state. In one study, researchers found that treatment of mastitis with topical curcumin significantly improved mastitis symptoms when measuring with the inflammation severity index. The inflammation severity index measures erythema (redness), breast tension, and reported pain.
Anti-inflammatory diets should be considered when working with clients who are struggling with recurrent mastitis or persistent subclinical mastitis.
So, what exactly is an anti-inflammatory diet? In clinical nutrition, anti-inflammatory diets combine the use of probiotic foods (like yogurt with live cultures, kefir, miso, sauerkraut), and prebiotic foods (steel cut oats, bananas, ground flax seeds, vegetables, legumes) with an avoidance of GI-irritating foods. GI-irritating foods can include foods with a high lactose load (ice cream, whole milk, soft cheeses), wheat, refined sugar (sucrose) and corn. It is important to note that not all dairy contains high lactose loads. Low-lactose dairy items include yogurt, hard cheeses, butter, heavy cream. Individuals who elect to keep dairy in their diet during an anti-inflammatory can focus on including low-lactose dairy.
The research that has investigated this diet (known as the IBD-AID) has been focused on alleviating signs and symptoms of GI inflammation. We also have population-level research that supports the ability of diet to modify markers of systemic (not just GI-specific) inflammation. Knowing this, it is possible IBD-AID may reach further than the GI tract.
While there is currently no peer-reviewed research to support the use of this (or any) anti-inflammatory diet to treat and/or prevent subclinical mastitis, oversight of an anti-inflammatory diet by a dietitian for individuals struggling with recurrent and/or subclinical mastitis may be be helpful with controlling the frequency and severity.
Filed under
Published on
Type a search + hit enter!
Browse the Blog
Category #1
Category #2
Category #3
Get Your copy →
Cross the finish line with confidence.
Don't walk into your IBCLC exam nervous - with our comprehensive study guide in your back pocket, you'll be prepared for every scenario and question.
© 2024 Hope Feeds Families LLC | Policies | Site Credit